Key Takeaways
Introduction
Higher blood pressure in the mornings is a common phenomenon experienced by many individuals. This article aims to explore the scientific reasons behind this occurrence, the implications for cardiovascular health, and potential strategies for managing morning blood pressure spikes. We will delve into the latest peer-reviewed research on circadian rhythms, the impact of lifestyle factors, and the effectiveness of blood pressure management techniques. By understanding the underlying causes and implications, readers will be better equipped to take appropriate measures for maintaining optimal health.

The Science Behind Morning Blood Pressure Spikes
Circadian Rhythms and Blood Pressure
Circadian rhythms are the natural, 24-hour cycles that govern our body’s internal clock. They play a significant role in regulating various physiological processes, including blood pressure [1]. Research has shown that blood pressure tends to be lower during sleep and begins to rise a few hours before awakening, reaching its peak in the early morning hours [2] as originally determined in the seminal study by Miller Craig et al. back in 1978. This increase in blood pressure is thought to be a result of the body preparing for the upcoming day’s activities, a process known as the “morning surge” [3].
One study found that the morning surge in blood pressure was more pronounced in individuals with hypertension and older adults [4]. Additionally, a higher morning blood pressure surge has been linked to an increased risk of cardiovascular events, such as heart attacks and strokes [5].
Lifestyle Factors Contributing to Morning Blood Pressure Increases
Various lifestyle factors can contribute to higher blood pressure in the mornings. These include poor sleep quality, sleep apnea, emotions and stress, high-sodium diets, alcohol consumption, and tobacco use [6] and level of physical activity undertaken. In a study examining the impact of sleep quality on blood pressure, researchers found that participants who experienced disrupted sleep had higher morning blood pressure levels compared to those who slept well [7].
Moreover, sleep apnea, a condition characterized by temporary cessations of breathing during sleep, has been associated with morning blood pressure spikes [8]. High-sodium diets can also lead to elevated blood pressure levels, as excessive sodium intake causes fluid retention, increasing the pressure on blood vessel walls [9]. Finally, both alcohol and tobacco consumption have been linked to higher blood pressure levels, with the effects being more pronounced in the morning [10].
Implications of Morning Blood Pressure Spikes for Cardiovascular Health
Increased Risk of Cardiovascular Events
As mentioned earlier, a pronounced morning blood pressure surge is associated with an increased risk of cardiovascular events such as heart attacks and strokes [5]. Research has shown that the risk of these events is higher in the morning hours, potentially due to the increased blood pressure levels and the body’s reduced ability to dissolve blood clots during this time [11].
One study found that individuals with a higher morning blood pressure surge were 1.7 times more likely to experience a cardiovascular event compared to those with a lower surge [12]. These findings emphasize the importance of closely monitoring and managing blood pressure levels, particularly in the morning.
Some people are referred to as ‘non-dippers’ who do not experience the normal nocturnal dip of 10-20% in blood pressure, while others may show really excessive morning surges. Both of these groups are found to generally have worse cardiovascular health, kidney problems and dementia risks associated with the changed patterns. About a quarter to a third of people with hypertension (high blood pressure) are ‘non-dippers’ seeing a less than 10% drop in blood pressure overnight compared to during the day, although people with normal blood pressure levels (normotension) can also be non-dippers and experience increased likelihood of organ damage as a result too.
Potential Consequences of Uncontrolled Morning Blood Pressure
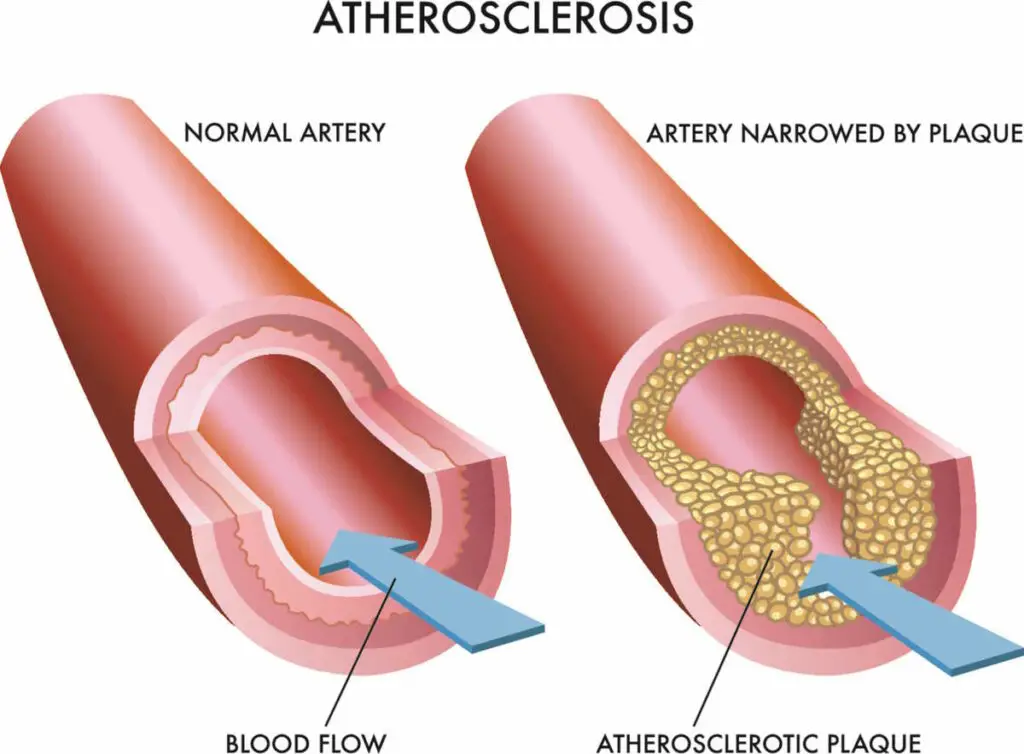
Uncontrolled morning blood pressure can have a variety of negative consequences on cardiovascular health. It can lead to the development or worsening of hypertension, which increases the risk of heart disease, kidney disease, and stroke [13]. Additionally, consistently high blood pressure levels can cause damage to the blood vessels and organs, ultimately leading to the development of atherosclerosis [14]. Atherosclerosis is the build-up of plaque in the arteries, which can restrict blood flow and increase the likelihood of heart attacks, strokes, and peripheral artery disease [15].
Furthermore, uncontrolled morning blood pressure can contribute to left ventricular hypertrophy, a condition in which the heart’s left ventricle thickens and loses its ability to pump blood efficiently [16]. This can eventually lead to heart failure and other serious cardiovascular complications [17].
Managing Morning Blood Pressure Spikes
Lifestyle Modifications for Improved Blood Pressure Control
Incorporating healthy lifestyle habits can be an effective way to manage morning blood pressure spikes. These include maintaining a balanced diet low in sodium, engaging in regular physical activity, limiting alcohol consumption, and avoiding tobacco use [18]. Additionally, improving sleep quality and seeking treatment for sleep apnea can help mitigate the effects of disrupted sleep on blood pressure [7], [8].
Stress management techniques, such as meditation, deep breathing exercises, and yoga, can also contribute to better blood pressure control [19]. By adopting these practices, individuals can work towards a healthier cardiovascular profile and potentially reduce the risk of morning blood pressure-related complications.
Pharmacological Interventions for Morning Blood Pressure Management
In some cases, lifestyle modifications may not be sufficient for controlling morning blood pressure spikes. In these instances, healthcare providers may recommend pharmacological interventions. Medications such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), calcium channel blockers, and diuretics can help lower blood pressure levels [20].
Some studies suggest that administering antihypertensive medications in the evening can be more effective in controlling morning blood pressure levels compared to morning dosing [21]. However, it is crucial to consult with a healthcare provider before making any changes to medication schedules or dosage.
Conclusion
In summary, higher blood pressure in the mornings is a common phenomenon that can have significant implications for cardiovascular health. Various factors, including circadian rhythms and lifestyle habits, contribute to morning blood pressure spikes. These spikes are associated with an increased risk of cardiovascular events and other health complications. Adopting healthy lifestyle practices and, if necessary, pharmacological interventions can help manage morning blood pressure levels and reduce the risk of associated health issues. It is important to consult with healthcare providers for individualized advice and recommendations based on personal medical history and needs.
References
- Hastings MH, Reddy AB, Maywood ES. A clockwork web: circadian timing in brain and periphery, in health and disease. Nature Reviews Neuroscience. 2003;4(8):649-61. link
- Smolensky MH, Hermida RC, Portaluppi F. Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Medicine Reviews. 2017;33:4-16. link
- Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107(10):1401-6. link
- White WB. The risk of waking-up: impact of the morning surge in blood pressure. Hypertension. 2006;47(2):137-8. link
- Muller JE, Stone PH, Turi ZG, et al. Circadian variation in the frequency of onset of acute myocardial infarction. New England Journal of Medicine. 1985;313(21):1315-22. link
- Pickering TG, James GD. Determinants and consequences of the diurnal rhythm of blood pressure. American Journal of Hypertension. 1993;6(3):166S-169S. link
- Lusardi P, Zoppi A, Preti P, et al. Effects of insufficient sleep on blood pressure in hypertensive patients: a 24-h study. American Journal of Hypertension. 1999;12(1 Pt 1):63-8. link
- Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. New England Journal of Medicine. 2000;342(19):1378-84. link
- He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database of Systematic Reviews. 2013;(4):CD004937. link
- Puddey IB, Beilin LJ, Vandongen R. Regular alcohol use raises blood pressure in treated hypertensive subjects. A randomised controlled trial. Lancet. 1987;1(8534):647-51. link
- Tofler GH, Brezinski D, Schafer AI, et al. Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. New England Journal of Medicine. 1987;316(24):1514-8. link
- Kario K, Ishikawa J, Pickering TG, et al. Morning hypertension: the strongest independent risk factor for stroke in elderly hypertensive patients. Hypertension Research. 2006;29(8):581-7. link
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115. link
- Celermajer DS, Chow CK, Marijon E, Anstey NM, Woo KS. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. Journal of the American College of Cardiology. link
- Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139-e596. link
- Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Annals of Internal Medicine. 1991;114(5):345-52. link
- Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. New England Journal of Medicine. 1990;322(22):1561-6. link
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Annals of Internal Medicine. 2002;136(7):493-503. link
- Goldstein CM, Josephson R, Xie S, Hughes JW. Current perspectives on the use of meditation to reduce blood pressure. International Journal of Hypertension. 2012;2012:578397. link
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Journal of the American Medical Association. 2003;289(19):2560-72. link
- Hermida RC, Ayala DE, Mojon A, Fernandez JR. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. Journal of the American Society of Nephrology. 2011;22(12):2313-21. link
You can check out any blood pressure reading and what it means on the xBloodPressure homepage.
Other Popular Articles:
